We’ve all either seen (and heard it happen), seen it on T.V, or had it happen to ourselves. Tearing an Anterior Cruciate Ligament (ACL) in the knee is one of those injuries where you just know it’s bad. If you’re an athlete, you can already see yourself sitting out the season, and if you’re Jane Average, the shock and trauma of having it happen to you is a little unbelievable. The sound is like a gunshot going off, and the pain is sharp and knife like through the whole knee. Up until that point in time, it’s likely that you would not have experienced such pain. Nothing can prepare you, and nothing can be done then and there…. YOU’RE OUT!
As soon as you hear the letters ACL about your favourite athlete, you know they’re out for the season.
As a practitioner, the connections we make with people are the things we value the most. So when we get an opportunity to help someone rehab after ACL surgery, we know there will be potential for a bond that will last a lifetime. As much as we are devastated for the person in front of us, we cherish the opportunity to help. And “help” is actually a light word in this situation. You’re doing much more than helping. When the trauma is so high, like the phoenix, the rise from the ashes is magnificent! It’s an honour and a privilege to bear a huge responsibility for that. You’re REBUILDING, RESHAPING and IMPACTING the whole person.
I do though want to make this point. What I’m about to describe to you is the way we do this particular ACL rehab for this injury. We believe it’s the best way forward. You may have done your ACL rehab differently with someone else, and the results you’ve gotten will be based on that. We are just giving you our experience.
Disclaimer: This is for Educational Purposes Only
Let me take a quick intercession to inform you as to the nature of our advice. We are experienced, healthcare clinicians. We wish to share our experience with you on topics to do with your health. We may be a little colourful in doing so, but at the heart of what we do is in-the-trenches experience. Whilst we have achieved academic success and understand the evidence, we are not solely evidence-based. We are, however, EVIDENCE INFORMED.
We find that the evidence is usually 10-15years (at minimum) behind what we are seeing in the clinic. We see real people, with real problems, and we’ve made a great living out of offering real solutions.
If all you’re after is the researched evidence, you can find some on Google Scholar, or you can very easily look for more on Google. We want to give you real-life advice, most of which you may not find in the research.
There is no way that this document can replicate or replace expert assessment and guidance given by a qualified registered healthcare practitioner who has seen you personally. I am sure you’re aware that I have no knowledge of your personal medical history or how you take care of your body. If you require care from a qualified practitioner, you would be best served by seeing someone who can empathise with your situation and treat you accordingly.
I’m sure you understand that I disclaim any and all responsibility for anything you do as a result of reading this document. And by reading this article, you accept 100% responsibility for the actions of you or anyone under your care.
The Surgery
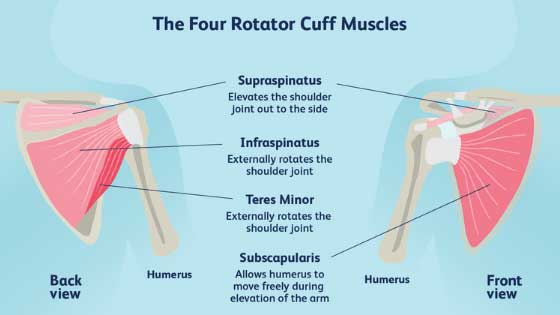
I’ll keep this short, simple and as easy to understand as I can make it. The ACL along with the PCL (Posterior Cruciate Ligament) make up a cross (X) like formation inside the knee and hold the knee together. The ACL stops the lower bone of the leg (tibia) from gliding too far forward from the upper bone of the leg (femur).
The surgery basically involves the surgeon drilling holes in both the upper and lower leg towards the inside of the knee, cutting out a roughly 20cm chunk of your hamstring, looping it over 4 times and inserting it into the drilled holes, replacing the torn ACL. They then screw that in and bone grafts around it to keep it stable.
Sounds nasty right? Well, it can be, depending on the surgeon. We have dealt with many of these injuries and rehabilitated thousands. And as routine as this surgery has become, there are still only a handful of surgeons in Sydney who I would trust with my own knee. The ACL rehab process is significantly easier in terms of time and quality of improvement when the surgery is clean and without complication. Ideally, the surgeon should be able to match the reconstructed knee as closely as possible to the feel of the healthy knee. Too loose, and the knee is unstable and likely to re-rupture, too tight and the rehabilitation is long, tough and painful. This means the surgeon needs to be highly experienced in the quantity of knees, but also getting a great quality of outcome. The operating procedures will look seamless and effortless, just as if he were performing a routine he has performed everyday, like brushing his teeth.
Providing you are fortunate enough to have this quality, the ACL rehab process should also flow seamlessly and you should see progress from day-to-day. If unfortunately, you have a poor surgical experience, your quality of the outcome will be reduced, as no amount of ACL rehab can hide a poorly reconstructed knee.

The ACL Rehab
The purposes of this article is to give you the information we have accumulated via our experience regarding the ACL rehab process after a knee reconstruction. The rehabilitation process is widely understood. There are many protocols and templates out there that pretty much follow the same path. These are generally evidence based and outline the return to sport based on a timeline, given that you reach your goals. We recommend the ACL Rehabilitation Protocol given by the North Sydney Orthopaedic Research Group, led by Associate Professor Leo Pinczewski, who is our preferred surgeon when it comes to the knee joint.
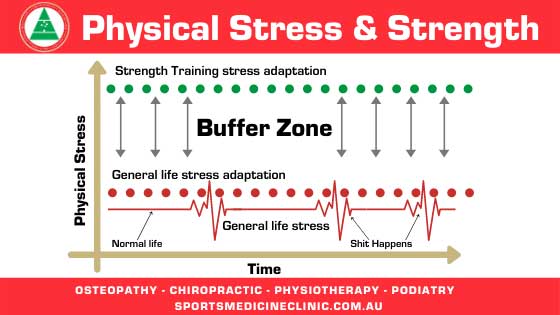
At the heart of this protocol, and this is why we advocate it, is this statement: “We recognize that GOAL based rehabilitation is far superior to TIME based rehabilitation…but biological healing must also be respected.”
We agree with this statement as it respects the body’s healing mechanism and understands that this healing of tissue is best achieved through reaching goals that are individualised. Time, being the same for everyone, is not individualised and what one person can do in 6 months another can’t do in 12 months. This rehabilitation protocol available for download, anyone can access it, but the information contained in it, is not the subject of our discussion today. What we are discussing today is the WAY this protocol is applied, and the considerations we take into account when figuring out HOW to apply it.
There are many patients who we have seen, that when looking at their protocol, one would think they would have a well rehabilitated knee. But upon examination, they are well short of their goals and expected outcomes, with associated pain, discomfort and weakness. This is not the fault of the protocol, but of the applicator, who has failed to apply the protocol within the framework of respecting the mechanics of the whole body, and respecting the tissue healing process.
Whilst the protocol we have advocated contains 6 phases, these phases are not distinct from each other. For example, Strength & Co-ordination begins in phase 2, but realistically, strength and coordination begins from phase 0 and is constantly continuing. So the applicator must allow these phases to seamlessly flow and understand when the components accelerate or back off. This might sound like a complicated task, but it need not be. If you’re using some basic principles to guide you, then the process becomes simpler and more effective.
Phased ACL Rehab principles
There are 2 major principles to consider when considering the phase progression:
- Are we respecting the tissues and where they are in the healing process? (Respecting the Tissue)
- Are we respecting the structure and function of the knee as it relates to the individual it’s attached to? (Structure & Function)
If these 2 principles are the first questions we ask ourselves each time we consult, then the process becomes simple and effective.
Phased ACL Rehab groups
I will summarise the phases into 3 groups:
Acute healing and Return to walking
- Here we are interested in reducing swelling and helping the wounds heal. So we use strategies like icing and elevation. We also follow the instructions from the surgeon as to wound care. We also must consider the hamstring that has been cut out, so we can begin some light activation of that tissue (Respecting the Tissue).
- Walking properly requires that we gain full knee extension at heel strike, so we must encourage full knee extension. This can be done by the therapist and can also be done at home by the patient (structure & function). It is imperative that you regain the full locking mechanism of the knee before moving forward (structure and function). This is where most rehab strategies fall apart. They move forward before full knee extension is achieved.
Improving Strength & Agility
- If you regain full extension of the knee, you are then able to fully recruit the quadricep muscles at full contraction, and recruit the hamstring eccentrically. Although strength has already started in return to walking, you can now accelerate the strength phase because you have respected where the tissues are in healing and you have regained a vital function of the knee joint.
- You can progress through strength based on pain feedback (Respecting the Tissue), by progressing through to multi-joint movements surrounding the knee (structure and function). Why do we do this? Because that’s the way the body works, in a system, not in isolated parts. So, you can begin squatting and deadlifting, using correct technique, progress through the movements based on pain feedback. You do the movement until it hurts, then BACK OFF a little to where it doesn’t hurt. The key here is that you the therapist, you move the joint a little more than previous and then you get the patient to engage that movement. Then the next time they see you, you go a little further. You respect the process and principles until you can do a full range squat and deadlift, then you begin loading.
- You then apply the same principles to agility. You begin slow and progress in pain-free range. By now the hamstring should have some solid healing and strength. Once you’re able to load a full range squat and deadlift, then you can begin running. The same principles apply here. Speed and direction will be based on pain feedback. Notice that pain is the feedback and not discomfort. Moving through new ranges will be uncomfortable for your body and your mind. But if the process has been followed, your strength and joint integrity will be better than your confidence will allow.
Return to Sport
- Whilst we appreciate that individual sports have their specific requirements, we believe that strength is strength. There is no football strong, or tennis strong. There is just STRONG relative to your body weight. Once you get strong, you then go and express that strength within your sport. So you need to have a certain amount of neuromuscular strength (Respecting the Tissue) before thinking about a return to sport or sport like activities.
- Most protocols require that you have at least 90% strength in the operated leg vs non operated leg. But if you were a weakling before your injury, you’re likely to be a weakling after it. So we want you to actually be of sufficient strength (structure and function) for your sport before attempting to go back.
- Just like strength training, you begin doing sports drills based on your tolerance levels. We want discomfort, but not pain. This will not only retrain motor patterns but also help you regain confidence. These drills should be sufficiently programmed so that there are incremental increases that move you to a return to full training capacity.
- Once you have trained enough to regain full confidence in your abilities to handle game situations (Respecting the Tissue), you may then consider competitive return to sport. But this full confidence must extend to strength, conditioning, and skill performance. If either of these are lacking, then a delay is advised (structure and function). This means that if you can’t perform all the tasks and skills required of you at full capacity, at the level required in that event, don’t play! You have no business returning to sport until you can.
The phases I have described will flow and melt into each other. If you follow the principles outlined, there should not be a backwards step. If you find that you have had to back off, then attention has not been paid to the tissues and the structure and function of the individual has not been considered before moving forward.
The last thing we want to see is a patient in the clinic, 2 years on from a knee reconstruction, with a knee that has limited extension and significantly reduced muscle mass… and they’re playing. That’s asking for trouble and a greater risk of re-injury.
This is a painful, painful injury, not to be taken lightly. The effects are on-going and long lasting. It is something you want to take seriously and make a priority. You definitely don’t want a weak, unstable knee moving into later adult life, and you certainly don’t want a second surgery. The difference between these things will be down to the quality of the surgery, of which you have less control, and the quality of the ACL rehab, of which you have more control over. Please see someone that is not just following a template. See someone who has sound principles that guide their treatment and whether you move forward or not. That will protect you. It could mean the difference between an old good knee and a bad one.
If you feel that any of the information we’ve given you here resonates with you and you feel we are in a position to help, please BOOK ONLINE as we would welcome the opportunity. If you feel that we can help you in any other way, please reach out to us via our CONTACT PAGE.

Dr. Sami Karam, Osteopath
I’ve been a qualified Osteopath since 2004. I’ve been playing football ever since I could remember and I have a passion for it. I’ve played at the highest level in the NSW State League at both Youth and Senior levels, and have also been Head Physician at numerous State League Clubs. I’ve travelled internationally and consulted with Sports academies in Barcelona and Italy. I have a special interest in Strength and Conditioning for footballers, as I believe it gives them an edge in their physical competition. My passion involves bringing all of this knowledge into every single treatment that I provide for all athletes. If you feel that I can help you and want to reach out to me, contact me.