Hand or elbow issues? It could be Golfer’s Elbow. Gripping things with your hands is about a basic human function as you can get. So when you get pain associated with gripping, the impact it has on what you can or can’t do is directly associated with how useful you are as a person. And since we all want to be useful (most of us), we need to address some of the main conditions that cause pain with gripping.
Such is the importance of the gripping function, people with amputated hands, fingers and/or nerve damage that reduces their gripping are often deemed “disabled.” Now before you go and start using the disabled car spaces, let’s just discuss how you’re able to overcome one of the main causes of painful gripping.
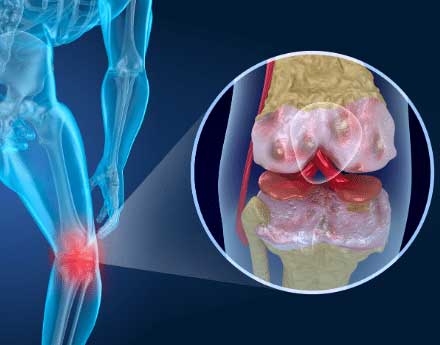
One of the common conditions that cause pain on the inside of the elbow is known as Golfer’s Elbow. The medical term for this is medial epicondylitis. This is generally characterised with pain that’s quite tender and achy and bruised to touch. It also feels quite tender and achy to grip and use your forearm.
Disclaimer: This is for Educational Purposes Only
Let me take a quick intercession to inform you as to the nature of our advice. We are experienced, healthcare clinicians. We wish to share our experience with you on topics to do with your health. We may be a little colourful in doing so, but at the heart of what we do is in-the-trenches experience. Whilst we have achieved academic success and understand the evidence, we are not solely evidence-based. We are, however, EVIDENCE INFORMED.
We find that the evidence is usually 10-15years (at minimum) behind what we are seeing in the clinic. We see real people, with real problems, and we’ve made a great living out of offering real solutions.
If all you’re after is the researched evidence, you can find some on Google Scholar, or you can very easily look for more on Google. We want to give you real-life advice, most of which you may not find in the research.
There is no way that this document can replicate or replace expert assessment and guidance given by a qualified registered healthcare practitioner who has seen you personally. I am sure you’re aware that I have no knowledge of your personal medical history or how you take care of your body. If you require care from a qualified practitioner, you would be best served by seeing someone who can empathise with your situation and treat you accordingly.
I’m sure you understand that I disclaim any and all responsibility for anything you do as a result of reading this document. And by reading this article, you accept 100% responsibility for the actions of you or anyone under your care.
So the movement that actually causes this is gripping. The main concern has to do with gripping and using your elbow and your wrist whilst you’re gripping. Movements like gripping and twisting, gripping and pulling, gripping and hammering, gripping and chopping will aggravate the inflammation. Anything that uses your wrist and your elbow whilst you’re gripping will tend to put strain on the tendons and cause them to get really swollen, inflamed and cause some pain at your elbow.
What happens is all these tendons on the inside of your forearm – the ones that close your fingers – attach onto one point on the inside of your elbow, called the Common Flexor Origin. As those tendons get tighter and tighter, and they pull on that bone, the bone will actually become inflamed. That will then add to your pain as well.
If you have had a Golfer’s Elbow condition for a relatively short period of time (2-6 weeks) the condition is considered to be fairly fresh and can be treated using some basic guidelines. This advice mainly relates to people who are suffering from this condition for a short period of time, and how they can help themselves or how we can help them to improve that condition.
The treatment that we may use for Golfer’s Elbow involves looking at this problem from a few different angles.
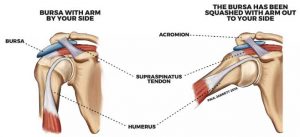
- This problem needs to be considered as an upper limb condition.
This means that you don’t just look at the elbow, you need to look at the wrist, the elbow, the shoulder, and the thoracic spine, and make sure that mechanically they’re all working well together. - The second strategy is you need to manage inflammation.
We can use ice, and we can use movement to actually help drain out inflammation and reduce inflammation in that area if we need to. - A third strategy that we need to implement is called load management. So we need to manage the kind of loads that we put on it.
We can’t overload it otherwise it will just keep getting inflamed and the process will repeat itself, but we can’t underload it because it will get weak.
So what you need to do is you need to find a point where you can do the work that you need to do, but not overload it. And then you gradually increase that load bit by bit, generally from week to week. Over time, that should help improve the actual condition. As the muscles don’t get weak, you can still function and the inflammation should die down gradually.
Now, some people will speak to me and say, “Well, look, I’ve had this problem for a good 3-4 months, it just doesn’t go away. I’ve seen a lot of people about it, it’s been going on for a long time, and I just can’t shake it.”
In these particular circumstances, there may be a lot of microtrauma at that particular area on the inside of your elbow, which means that every time you use it, you increase that microtrauma.
The strategy that we need to implement to actually overcome this is quite painful. It’s not nice, and it requires that we go in there and actually really work hard on the inside of that elbow and create some hyper inflammation. What that will do is it will bring on a cascade of events where your body will actually try and heal that area.
So previously, your body was in a state of chronic inflammation and some kind of tissue thickening that it just wasn’t getting out of. When we go in there, we beat it up, your body thinks that you’ve just hurt yourself, and that starts to repair the area. So we need to be a little bit firmer with you, and maybe a little bit painful, but we get to a point where it’s really hyper inflamed and it’s really swollen and then we ice it back down.
We basically get you to the point where the strategies I discussed earlier with you when this is a short term problem become applicable. When that happens, the tissue should repair quite well and you’ll find that your pain reduces quite significantly. No need for forearm straps, wraps or any kind of device.
Follow these Golfer’s Elbow guidelines when you feel that pain on the inside of your elbow is making you less useful than you’d like to be. Because we’d prefer that you be useful, and not take the disabled car spaces from those people who actually need them.
If you feel that any of the information we’ve given you here resonates with you and you feel we are in a position to help, please BOOK ONLINE as we would welcome the opportunity. If you feel that we can help you in any other way, please reach out to us via our CONTACT PAGE.

Dr. Sami Karam, Osteopath
I’ve been a qualified Osteopath since 2004. I’ve been playing football ever since I could remember and I have a passion for it. I’ve played at the highest level in the NSW State League at both Youth and Senior levels, and have also been Head Physician at numerous State League Clubs. I’ve travelled internationally and consulted with Sports academies in Barcelona and Italy. I have a special interest in Strength and Conditioning for footballers, as I believe it gives them an edge in their physical competition. My passion involves bringing all of this knowledge into every single treatment that I provide for all athletes. If you feel that I can help you and want to reach out to me, contact me.