Will a corn go away by itself?
Corns may not go away on their own, especially if the cause of the corn, such as repetitive friction or pressure, persists.
Corns develop as the skin’s natural response to protect itself from these forces, and they often require intervention to resolve. Without addressing the underlying cause and providing appropriate care, corns can persist and potentially worsen over time.
In some cases, if the source of friction or pressure is eliminated, a small corn may gradually diminish on its own as the skin reverts to its normal state. However, this is not a guaranteed outcome, and larger or more established corns often require active treatment.
It’s essential to manage corns promptly to prevent them from becoming more painful and problematic. If you have corns that are causing discomfort or concern, it’s advisable to consult a podiatrist or healthcare professional for proper evaluation, treatment, and guidance on preventing their recurrence.
What happens if you leave a corn alone?
If you leave calluses and corn untreated, they can become thicker and more painful over time.
This is because the thickened skin can continue to build up in response to the pressure and friction that caused the callus or corn in the first place.
In some cases, the thickened skin can become so severe that it develops into an ulcer or a sore. This can be particularly dangerous for people with diabetes or other conditions that affect circulation or the immune system, as it can increase the risk of infection and other complications.
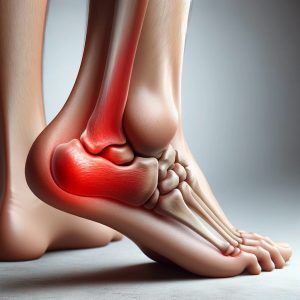
In addition to causing pain and discomfort, untreated calluses and corns can also affect your gait and balance, making it more difficult to walk or stand comfortably. This can lead to other foot problems, such as plantar fasciitis, heel spurs, or ankle sprains.
Overall, it’s important to seek treatment for calluses and corns, particularly if they are causing pain or interfering with your daily activities. A podiatrist can provide an accurate diagnosis and recommend appropriate treatment options to help you manage the problem and prevent complications.
How long does it take a corn to go away on its own?
The time it takes for a corn to go away on its own, if it goes away at all, can vary widely depending on factors such as the size of the corn, the underlying cause, and individual differences.
In some cases, small and soft corns may gradually diminish on their own if the source of friction or pressure is eliminated. This may take weeks to months.
However, it’s important to note that many corns do not go away on their own, especially if they are larger or more established. Corns often persist and may even increase in size if the contributing factors, such as ill-fitting footwear or structural foot issues, are not addressed. In such cases, active intervention is typically necessary to resolve the corn.
The best approach to managing corns is to identify and address the root cause, alleviate the pressure or friction, and consult with a podiatrist to effectively reduce the thickness of the callus/corn and remove it. Seeking professional guidance is important for effective and timely management of corns, as well as preventing their recurrence.
What happens if a corn is not removed?
Leaving a corn untreated and allowing it to persist can lead to several potential consequences and complications, including:
- Pain and Discomfort: Corns are often painful, especially when they are subjected to pressure or friction. Neglecting treatment may lead to increased discomfort and pain during activities like walking or wearing certain shoes.
- Enlargement: Corns may continue to grow and increase in size if the source of pressure or friction is not addressed. Larger corns can be more painful and harder to treat.
- Changes in Gait: To avoid putting pressure on a corn, individuals might unconsciously alter their walking pattern. This can lead to issues with gait and posture, potentially causing pain in other parts of the body.
- Risk of Infection: Corns can cause the skin to crack, creating an entry point for bacteria. This can lead to infection, which may require medical treatment.
- Chronic Discomfort: Corns that persist over time can become chronic sources of discomfort and inconvenience. This can affect one’s quality of life and mobility.
- Complications for Vulnerable Populations: For individuals with diabetes or circulatory problems, the risk of complications related to untreated foot conditions, including corns, is heightened. These complications can be more severe and challenging to manage.
Worsening Skin Health: Neglecting foot care can result in worsening skin health, making the skin more susceptible to other issues, such as fungal infections.
Given these potential complications, it’s advisable to address corns promptly with proper treatment or preventive measures. Consult a podiatrist or healthcare professional for guidance on the most suitable approach to manage and prevent corns effectively.

Dr. Yasmin Karam
Dr. Yasmin Karam graduated with a Bachelor of Health Science/Masters in Podiatric Medicine. Dr. Yasmin has had experience working in both private and public sectors, exposing her to a great range of foot complications; from minor nail and skin pathologies to foot mal-alignments and diabetic foot ulcers.