Whiplash injury can be a result of sudden and unexpected force applied to the neck or back. There are thousands of cases of whiplash every year and many of which are caused by car or motorbike accidents. This post will give an overview of whiplash in general, as well as different causes, symptoms, diagnoses and treatments for whiplash injuries.
What is whiplash?
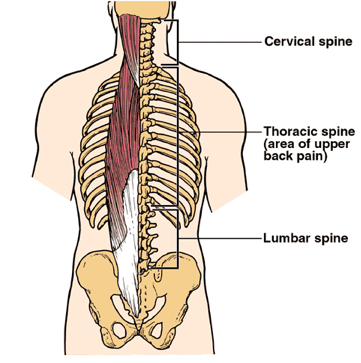
Whiplash can occur when the lower back or neck undergoes a sudden contraction of the spine. People with whiplash can have a harder time controlling their internal muscles and tend not to be able to properly support their own weight or that of another person.
In many cases, a patient will have whiplash pain caused by a muscle or ligament that has been stretched beyond its normal range of movement. The cause of this pain might be a combination of poor movement patterns, misuse of joints, and even physical trauma from riding a bike or driving.
Whiplash causes
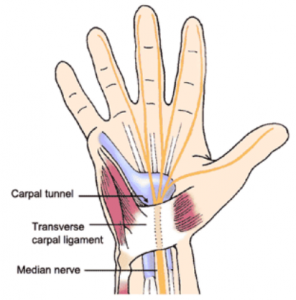
The neck and spine are a complex network of muscles and bones that control movement and help us think and remember. Injury can damage the connective tissue that holds these tissues together. This type of injury may cause numbness, tingling and sharp pain.
There are a number of causes of whiplash injury, these might include:
- Automotive accidents
- Injuries caused by collisions
- Contact sports
- Motorcycle accidents
- Extreme sports
- Crash landings
Automotive causes of whiplash
Whiplash in automotive settings can be the result of sudden and sharp movements, such as hitting the side of the steering wheel after a car crash. The key term is “sudden” sharp movements, such as hitting the side of the steering wheel after a car crash. When the neck and spine bend and turn violently, you might experience the condition as a whiplash injury.
For instance, it might occur when you fall off or ride a motorcycle in a hard corner. You may have whiplash injury in a car or motorcycle if:
- Your car goes out of control while you’re driving
- You experience a sudden turn, a bump or a jolt
- You experience a sudden stop
- Your car suddenly collides with another car or stationary object
Whiplash in sportspeople
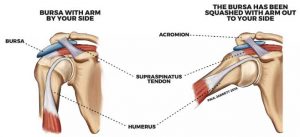
Whiplash is a surprisingly common injury that many professional sports players deal with repeatedly. When this happens to the ligaments in the neck or upper back, the result can be pain that can be very debilitating and costly to the athlete.
Whiplash is considered one of the most common sports injuries. It usually happens to the neck and upper back, but it can also happen to the shoulder and arm. One of the reasons for this is because it involves rotational forces that are causing the joint to move in a twisting or turning motion.
How can you prevent a whiplash injury?
As we age, our muscles become weaker and less flexible and so whiplash can get worse. Muscle spasms may occur due to muscle fatigue, which may increase the risk of whiplash. No matter how careful you are, accidents can still happen.
Be careful when you drive your car
Take extra care when you drive and avoid doing anything that could cause a whiplash injury. Here are some suggestions that may help reduce risks:
- Ensure that diagonal seat belts are securely fastened
- Backhand turns and jerky driving are more likely to lead to whiplash injury
- Avoid driving while you’re tired or fatigued
Neck strength for contact sports
Strengthening the neck is vitally important for athletes involved in collision sports. Not only does it help with reducing whiplash injuries, but improves outcomes associated with concussions.
Symptoms of whiplash
So, what are the signs and symptoms of whiplash?
If you have whiplash, you might have pain, weakness, and stiffness in your neck and arms, especially in the lower back and neck. You might also be experiencing headaches, neck pain, and discomfort or numbness in the lower back.
Is whiplash permanent?
When you’re injured in a car accident, you may experience whiplash. This is a severe type of pain that manifests after your neck is jolted by a sudden impact with a vehicle. If you experience this pain regularly, it can be hard to tell if it’s temporary or permanent. You should consult with a healthcare provider to assess and diagnose.
How whiplash is diagnosed?
Most of the time, whiplash is a symptom of another injury, such as whiplash in car accidents. The doctor or healthcare professional may try to pinpoint the cause of the whiplash injury. If you’re suffering from whiplash, you can avoid a lot of hassle by knowing how to identify and treat whiplash injury.
Transverse rib injury and Pit Bull Syndrome
The word “whiplash” can be a misleading term, as it has been used to describe a wide range of different injuries. Another term used might be “transverse rib injury”, which can more precise because it better reflects the actual condition of the injury. Whiplash includes any rib or vertebra injury and is also known as a “vertical neck fracture” or “vertical transverse rib fracture.” The condition most commonly associated with whiplash is the infamous “Pit Bull Syndrome” (often abbreviated as PBS).
Diagnostic tools
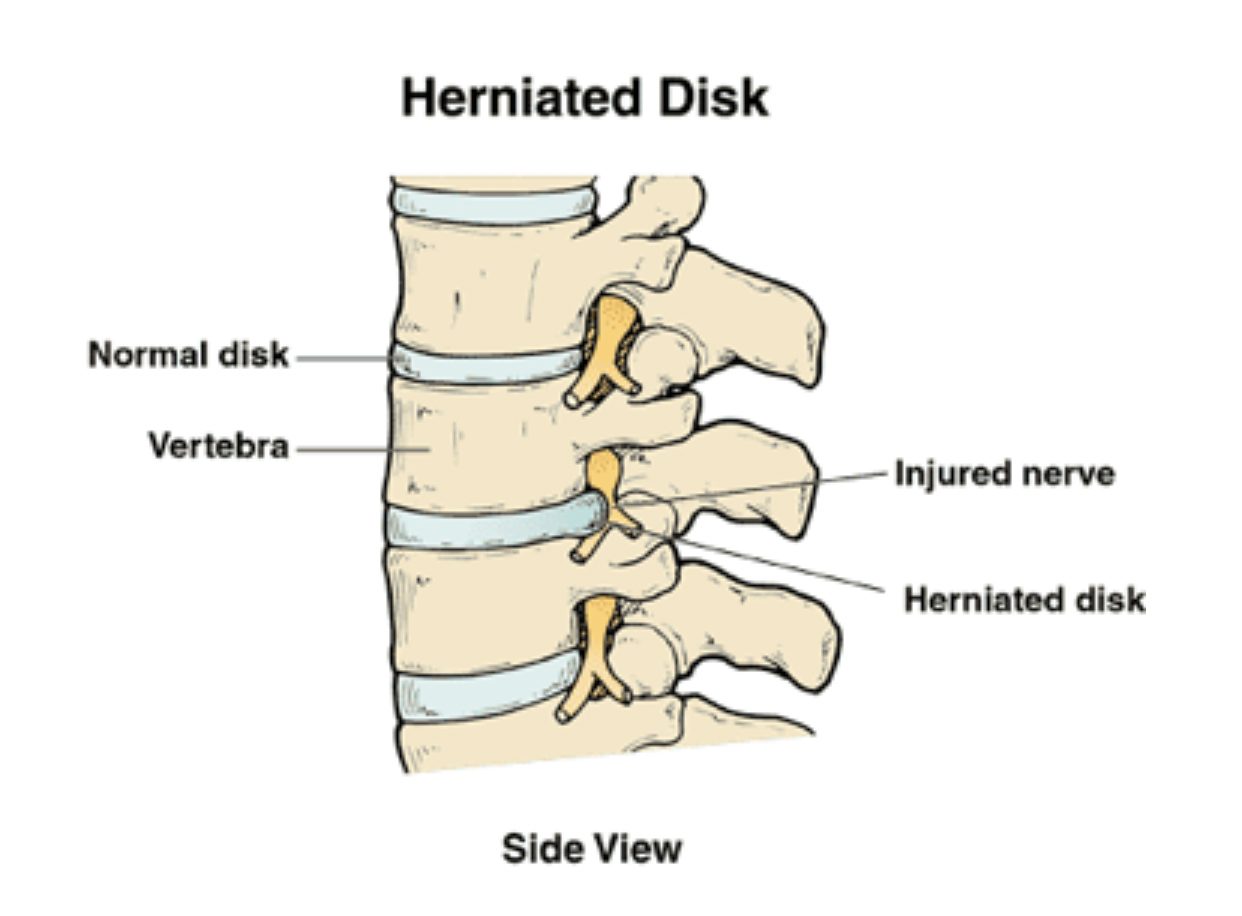
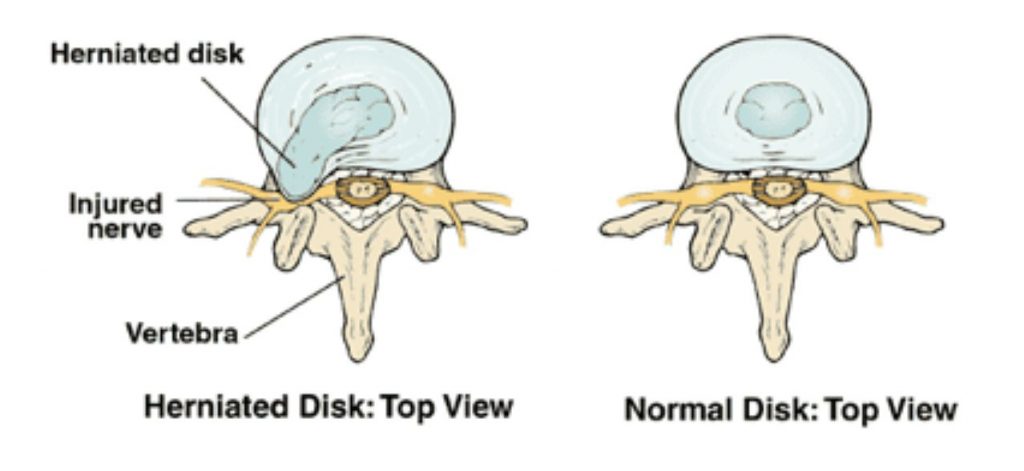
X-rays, CT Scans and MRI may show the spine, or any vertebrae, flexing and twisting. This tool may show a disc protruding from between the vertebrae, which may be evidence of whiplash injury.
In addition, a CT scan is a helpful diagnostic tool. It can help detect herniated discs and blood clots, among other things.
Physical examination
Baseline physical examination may also be conducted to find out if there are any immediate problems. This will help in ruling out any further injury or issue that is related to the injury.
Sensory evaluation and testing are also done to diagnose the injury. The severity of the injury, pain and immobilization on the neck is assessed by the doctor. Steps of this exam may include moving your neck and back in particular positions and medical teams detecting any numbness, tingling or any other signs of disc protrusion.
Treatment for whiplash
There are several treatment options to treat whiplash injuries. The standard treatment for whiplash may include physical therapy and the use of pain medications like Voltaren and Ibuprofen. But this often leaves the underlying mechanical issues unresolved.
Other treatment options by medical teams can include spinal adjustments, sports medicine, physiotherapy, dry needling, chiropractic treatment, massage, and osteopathy. All these treatments may treat the problem, the underlying mechanical trauma, and prevent future complications.

Dr. Sami Karam, Osteopath
I’ve been a qualified Osteopath since 2004. I’ve been playing football ever since I could remember and I have a passion for it. I’ve played at the highest level in the NSW State League at both Youth and Senior levels, and have also been Head Physician at numerous State League Clubs. I’ve travelled internationally and consulted with Sports academies in Barcelona and Italy. I have a special interest in Strength and Conditioning for footballers, as I believe it gives them an edge in their physical competition. My passion involves bringing all of this knowledge into every single treatment that I provide for all athletes. If you feel that I can help you and want to reach out to me, contact me.